HEALTHNIC
My year-long thesis project sought for the meaning of patient experience, essential elements of excellence in patient experience, and explored the ways they can be utilized, improved, and intervened.
an explorative journey that strived to uncover the essential elements of excellent patient experience.
an empathetic journey to discover effective intervention points within their experience.
a user-centered journey of validating hypothesis and refining prototypes through testings.
Journey
What is patient experience, and how can it be improved?
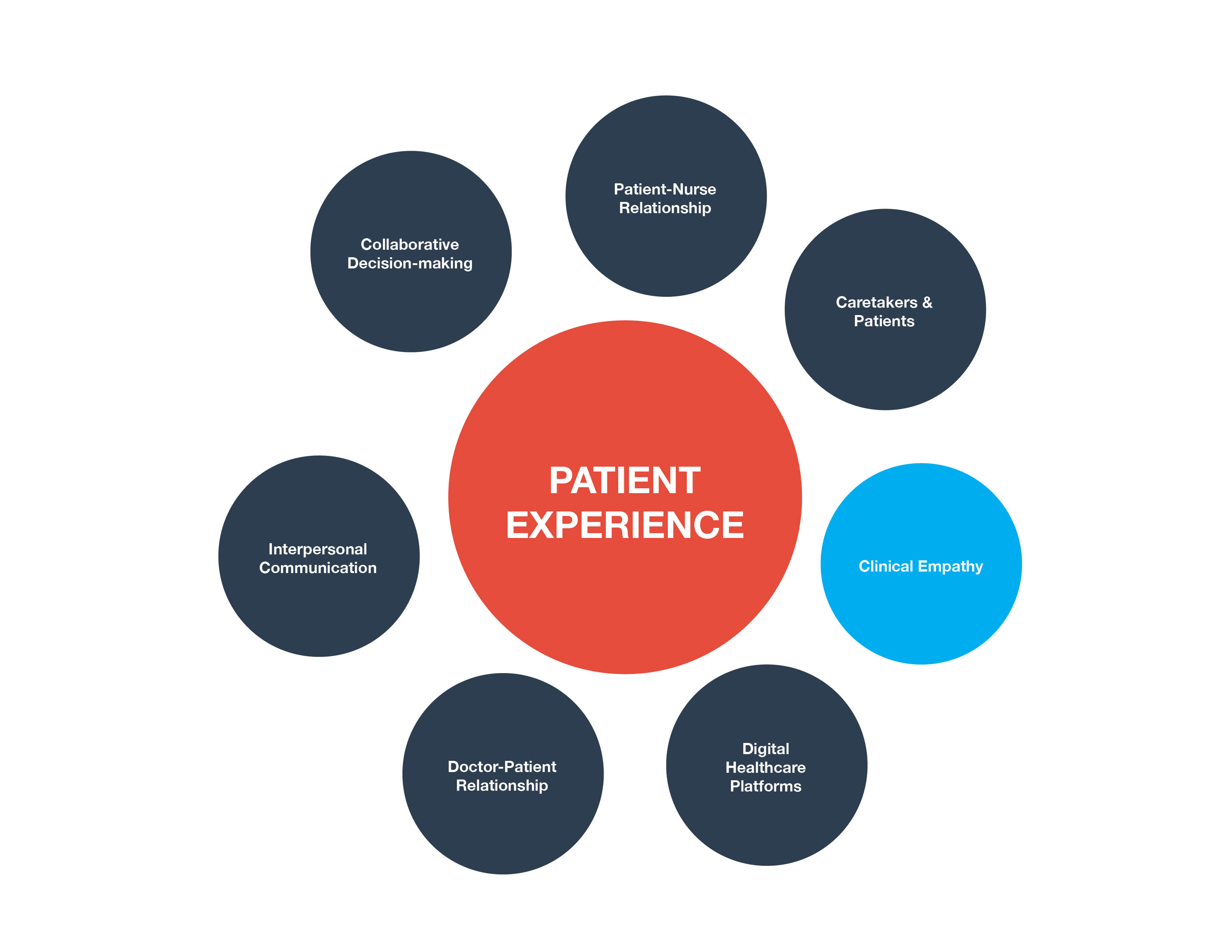
Patient experience is a complex web of ecosystems with a multitude of stakeholders and interactions. But as I researched into the main topics around patient experience, a recurring keyword kept on appearing – clinical empathy. Better patient experience derives from the better relationships between patients and medical staff and better relationships come from empathetic communication.
“Cognitive and behavioral attributes that involve the ability to understand how a patient’s experience and feeling and are influenced by their symptoms and illness and the capacity to communicate this understanding to the patient.”
– Hojat, 2002
There have been vastly different definitions of the term clinical empathy throughout medical history. Most recently, researchers began to define practicing clinical empathy as possessing the ability to understand patient’s emotion then communicate the understanding back to the patients to subtly inform that they care and respect patient’s emotions.
Interviews
I interviewed several medical professionals and experts on clinical empathy training. In our conversations, I asked them about how they define clinical empathy, their opinions on the subject, as well as their hopes and regrets within their professional experiences thus far.
One thing that stood out to me was the polarized opinions on the practice of clinical empathy. Dr. Back stated that time should not be an issue to properly practice clinical empathy since it is about asking the right questions and having the right skills. While others stated they wished they could have spent more time with patients to establish a better and more empathetic relationship with them.
Ethnographic
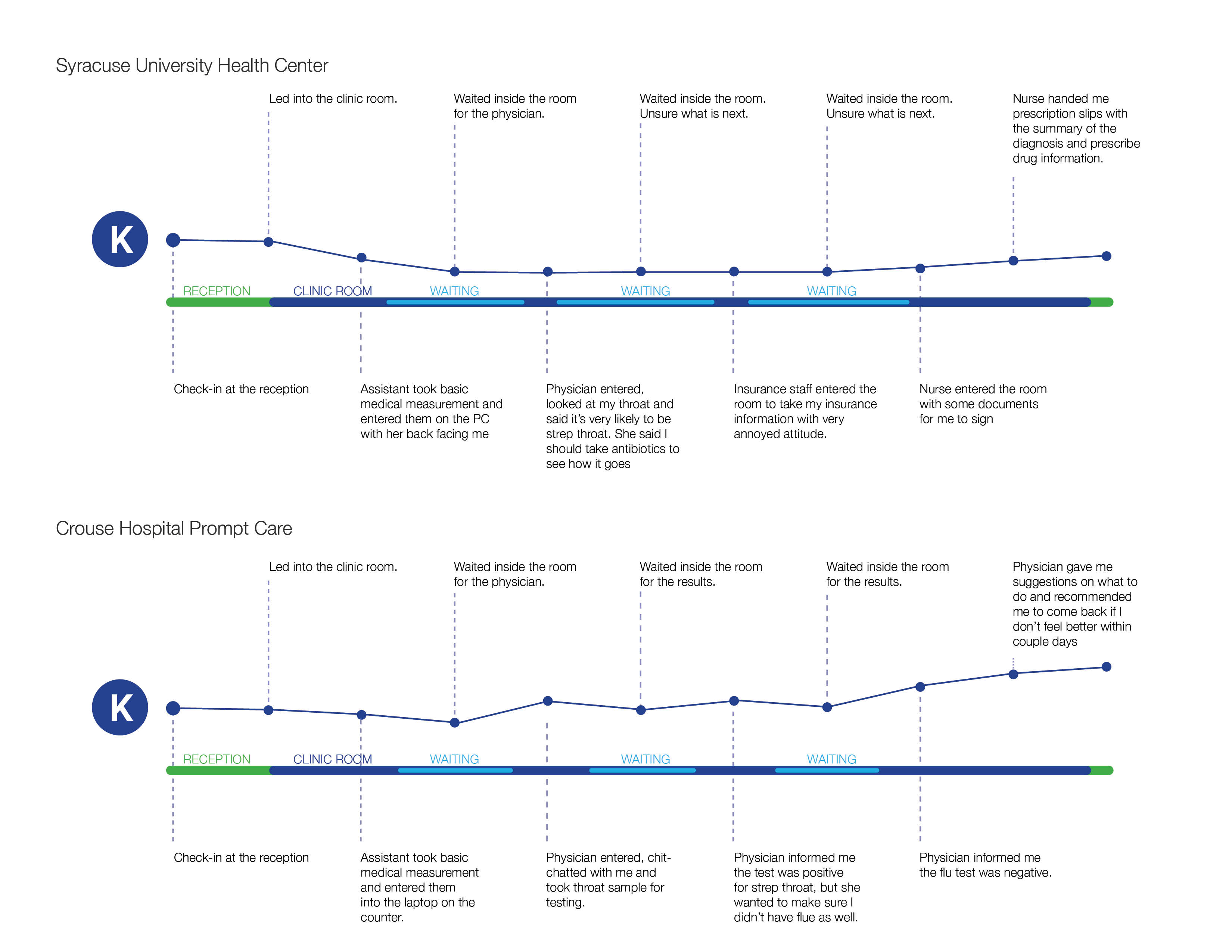
During my research, I was ill twice with strep throat. I purposefully chose two different healthcare facilities in order to examine the successes and pain points of two different experiences personally.
The experience at SU Health Center was considerably better than the one at Crouse Promptcare. The SU physician was approachable and caring about my symptoms. She chatted with me about topics other than my medical condition and gave me further medical instruction while the physician at Crouse Promptcare only briefly discussed with me then prescribed me antibiotics. The entire visit lasted under 5 minutes.
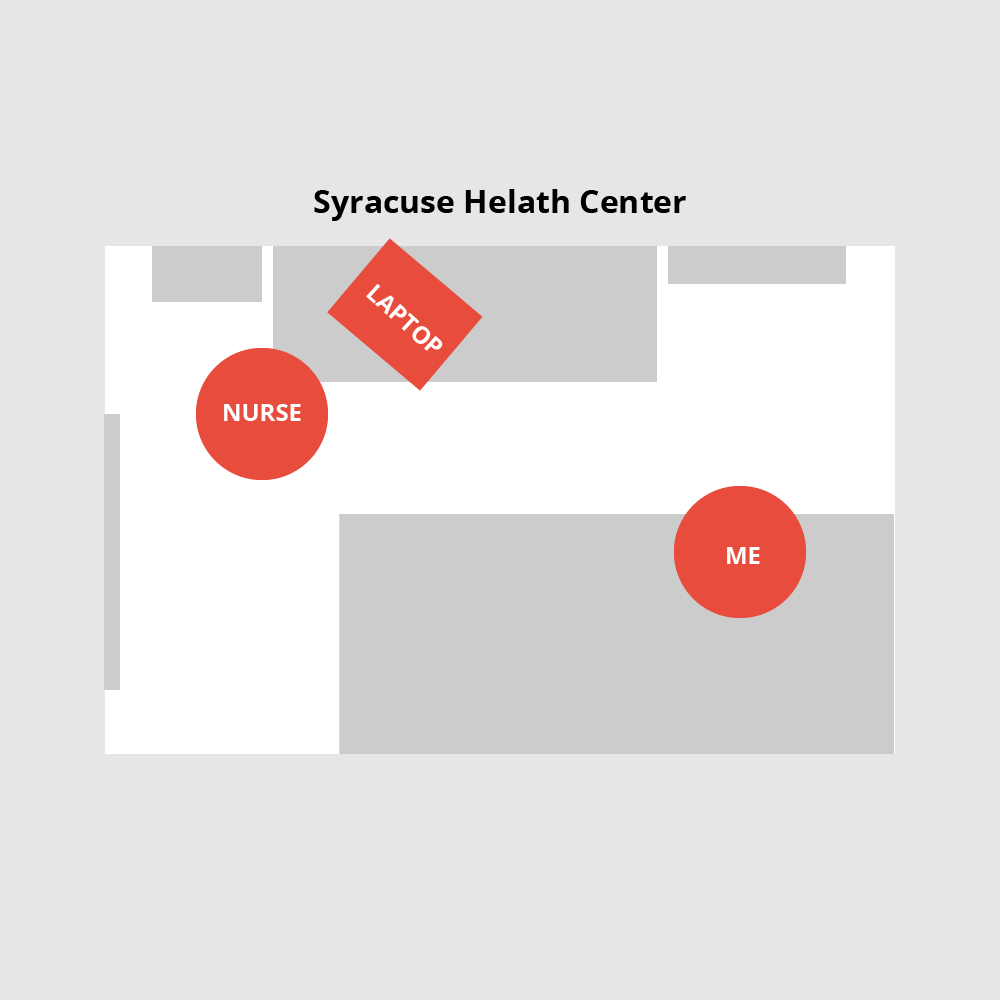
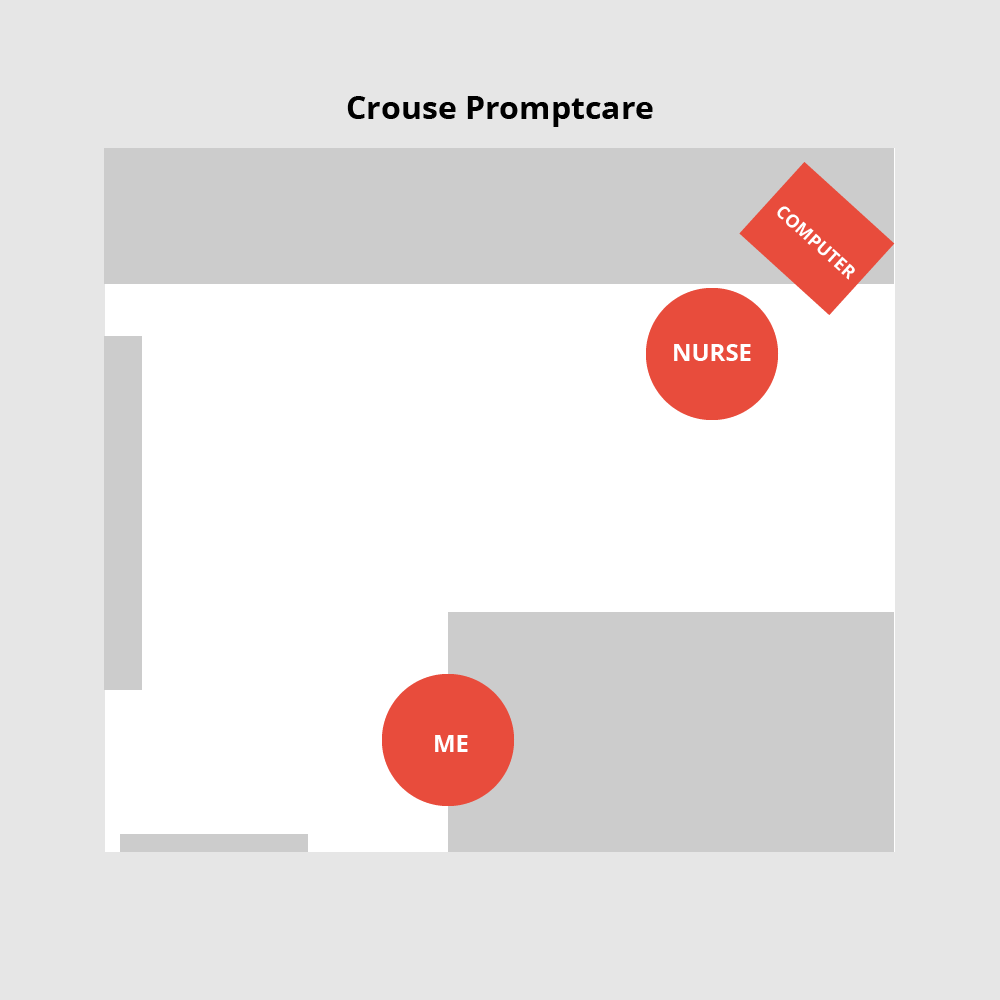
The layout of the clinic room also made a great difference. At the SU Health Center, the position of the computer allowed the physician make eye contact with me while periodically. At Crouse Promptcare, the physician's back was facing me for the majority of the time.
Competitive Analysis
Beyond medical and nursing schools, there are only a handful of services that provide clinical empathy training.
Vital Talk and Oncotalk both focused on physicians who treat patients with end-of-life illness, while Empathetics focuses on general medical staff and management as well.
They also employed different formats of training. Vital Talk, and Oncotalk utilize in-person seminars, while Empathetics utilized application-based training and in-person consultation for hospital management.
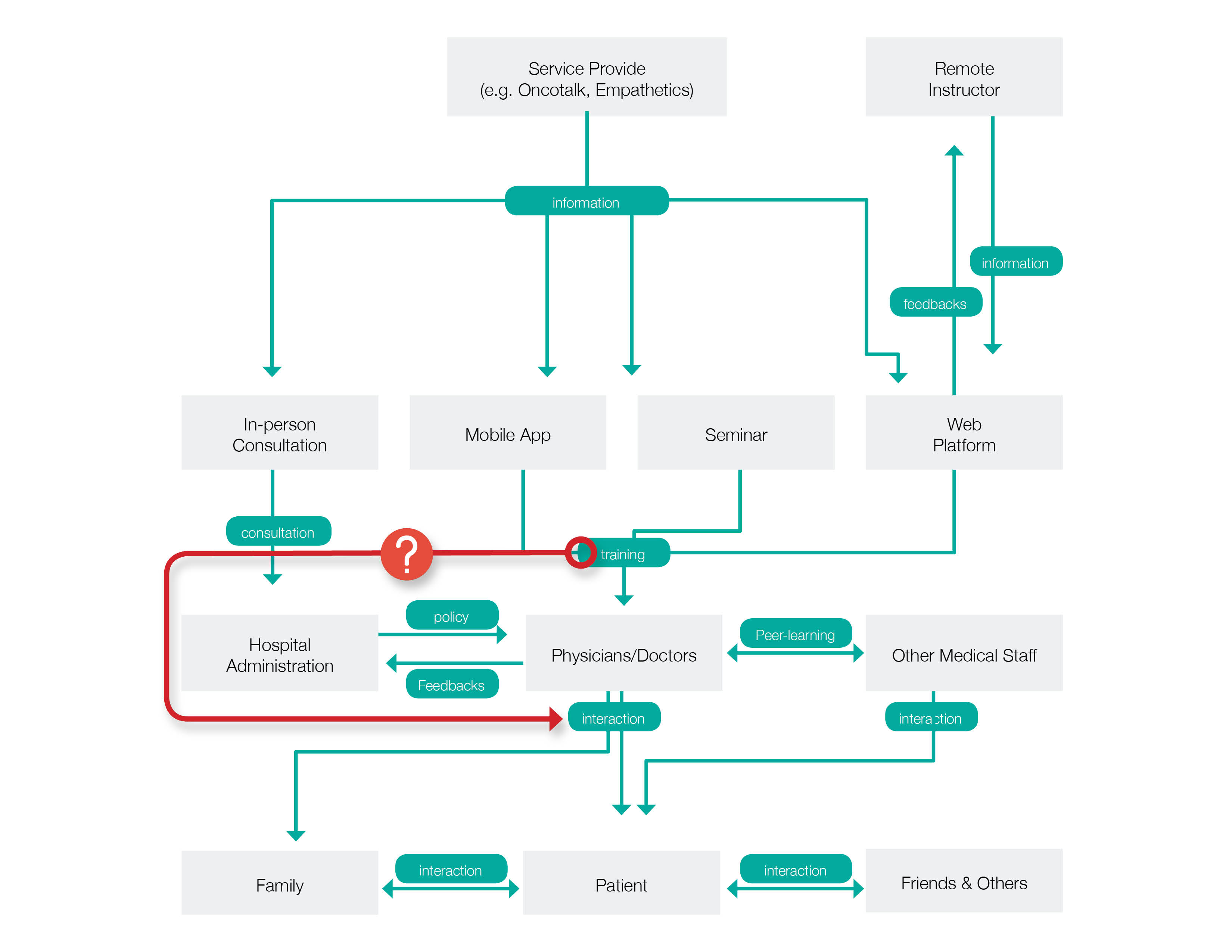
Service Map
The service map of current clinical empathy training programs outlines the interactions, and the exchange of information between their physicians, other medical staff, and patients. It is possible to improve the knowledge and techniques of practicing clinical empathy within the structure, yet there is currently no system implemented to ensure and measure the practice of clinical empathy in an actual clinical environment.
It is doubtful that the training of clinical empathy can increase the frequency of practicing it in an actual clinical environment. Even though they claimed their programs have shown promising results, other studies have pointed out the summative assessments were done shortly after the training in the controlled environment. There was no evidence suggesting the training would have a lasting effect on the actual clinical environment.
Clinical empathy is an essential element in improving patient experience, and clinical outcomes. However, it is not commonly practiced due to restraints such as time, perception, and lack of training.
Even though research has stated that clinical empathy can be trained, there is no evidence suggesting the long-lasting effect of it on physicians. Current training system lacks ongoing engagement that can encourage, motivate, and remind physicians the importance of clinical empathy and promote the practice of it within the real-world clinical environment.
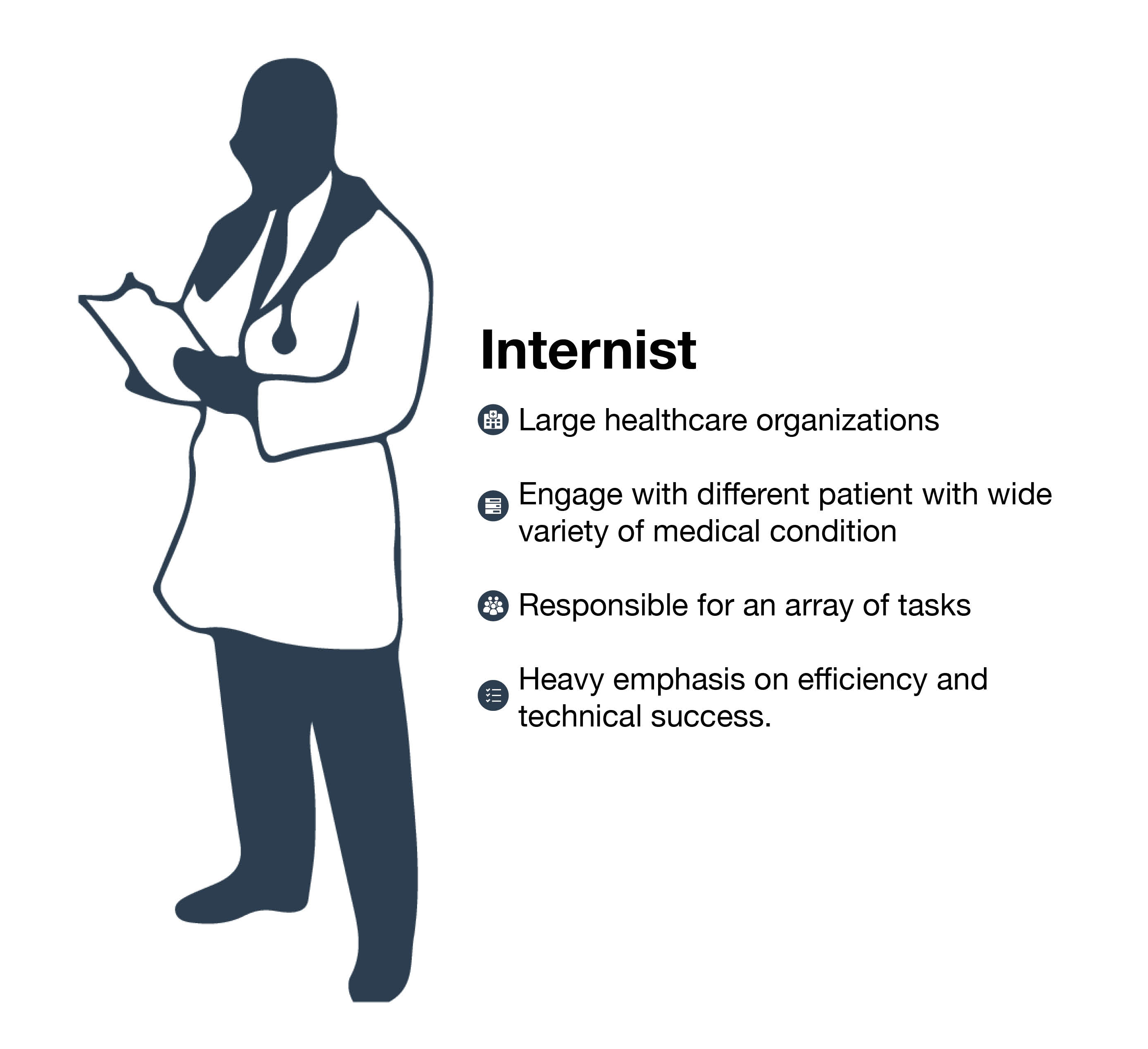
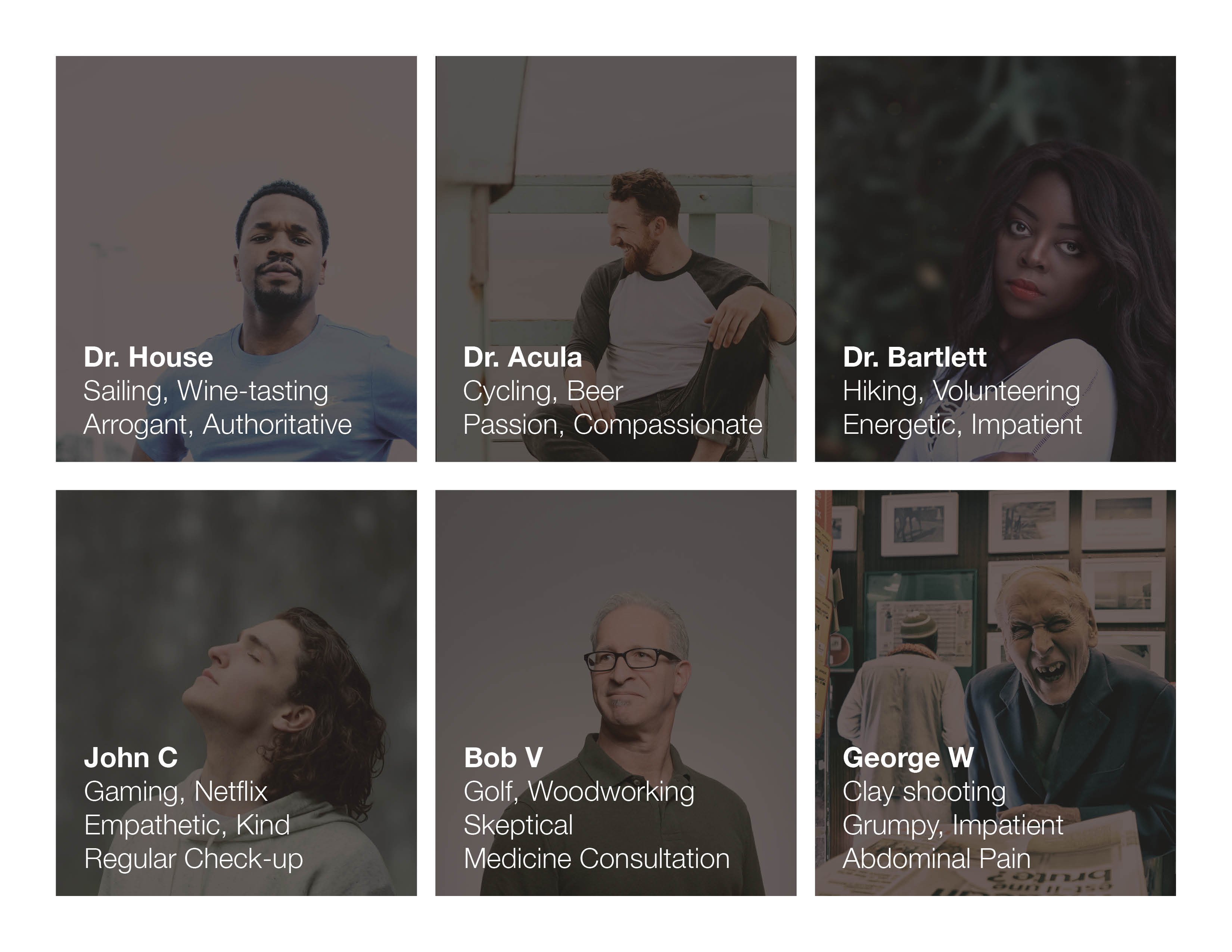
Target User
The target users are the internists that see out-patients within large healthcare organizations.
Usually, it would be fairly challenging for internists to establish strong interpersonal relationships with their patients since they engage with different out-patients every day and their wide level of medical expertise engages with patients who suffer from various of medical conditions. Since they are working within large healthcare organizations, they are usually under pressure from upper management about their efficiency and outcomes.
The selected target users group certainly made the project more challenging, yet I believe they are the ones who would benefit the most from the scope of this project.
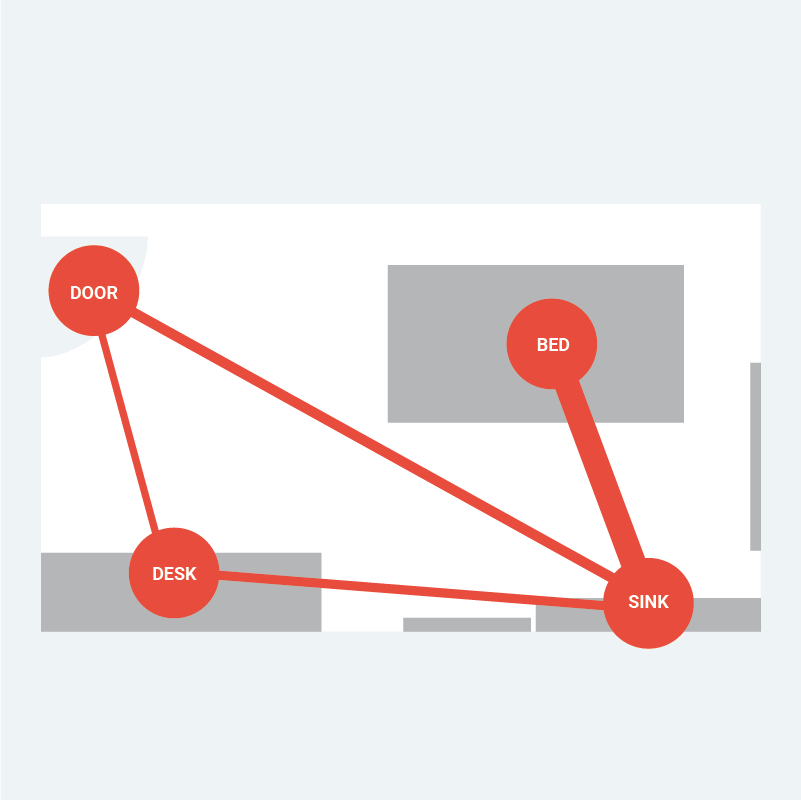
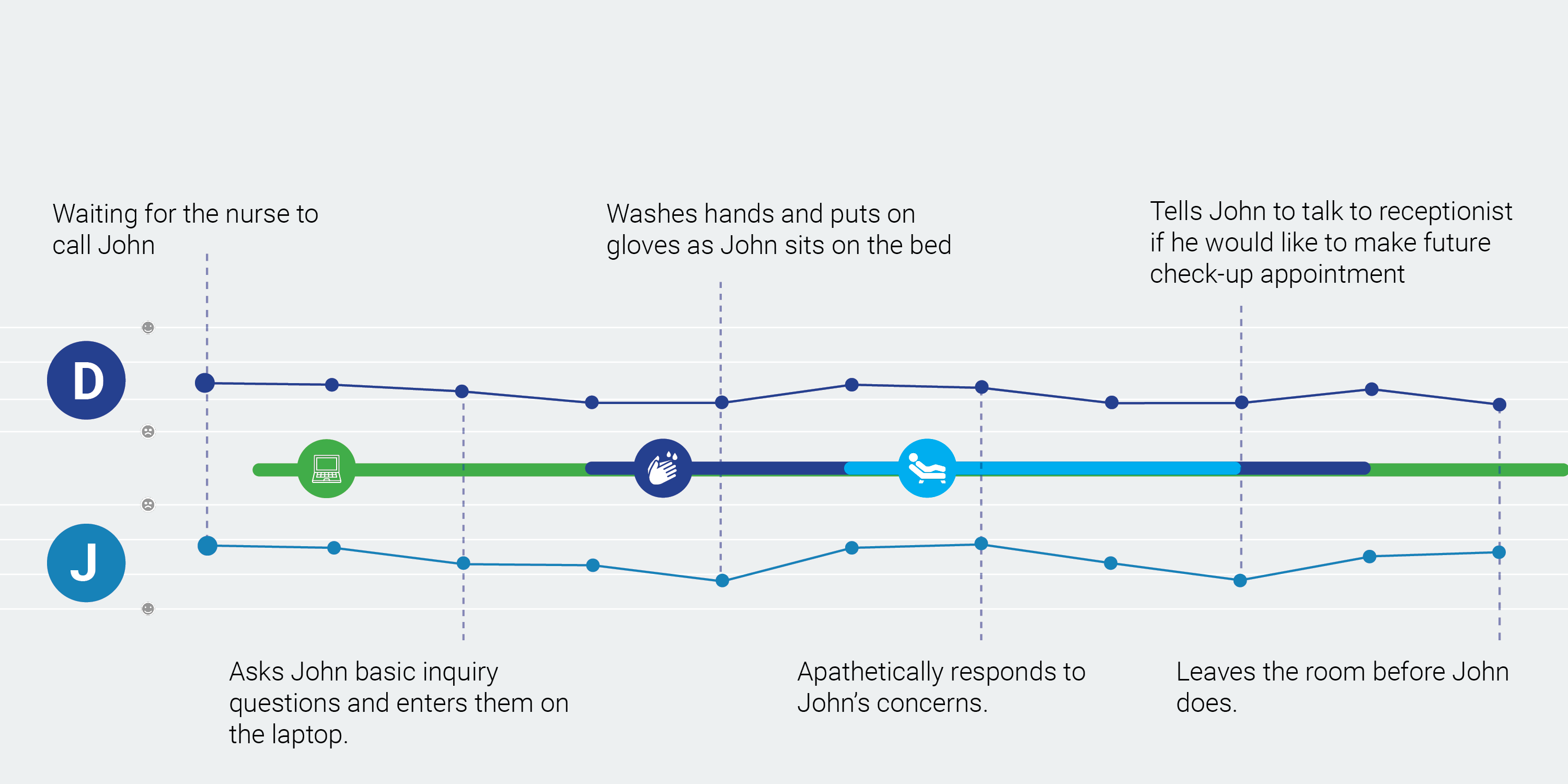
Journey & Behavioral Map
With 3 physician archetypes and 3 patients ones, I created different possible journey maps detailing their interactions, moods, and locations of their respective experience.
I then organized the data from the experience map and created behavioral maps based on the foot traffic, mood, and time spent within the room to understand where some potential intervention points might be that can be utilized to affect physicians’ daily workflow to remind and motivate them to practice clinical empathy.
Touch-points
I then selected 5 potential touch points based on the map then brainstormed how that can be utilized to subtly intervene in a physician’s daily workflows to subtly encourage and motivate the practice of clinical empathy.
The criteria of the touch-points include having a large influence on the patient's experience in the clinical space and being frequently engaged with physicians and/or patients.
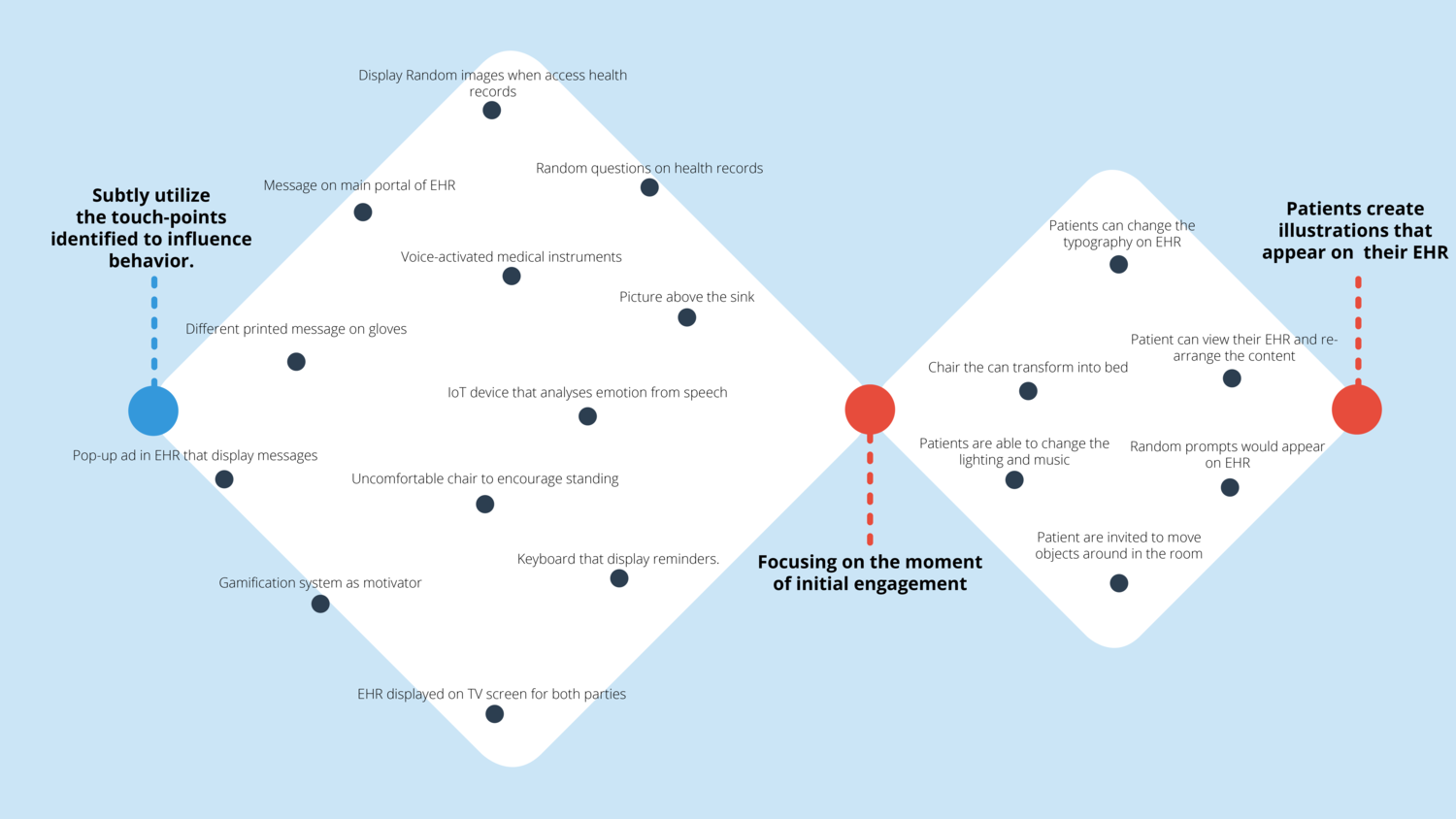
Brainstorming
I wanted to utilize the touch-points in a subtle, psychological, and un-disruptive way that would affect the physician’s workflow without being authoritative or telling them what to do. I then began to conceptualize how those touch-points can be modified to bring minor inconvenience into their workflows in order to bring individuality into every interaction with the patients.
In the beginning stage of brainstorming, I challenged myself to come up with crazy, seemingly impossible ideas, then build upon, modified, or altered them to be more suitable for reality.
The Moment
With the feedback I had received and the progress of building up these ideas, I gradually shifted focus from using certain physical touchpoints to change one specific moment within patients’ experience in the clinical room.
The specific moment is when physicians first gain the impression of the patient. For this instance, it would be when physicians are reading patient’s EHR and when a physician first enters the room. Instead of the standardized health records that simplify patients down to just numbers and descriptions, I wanted to transform health records to represent the individuality of each patient.
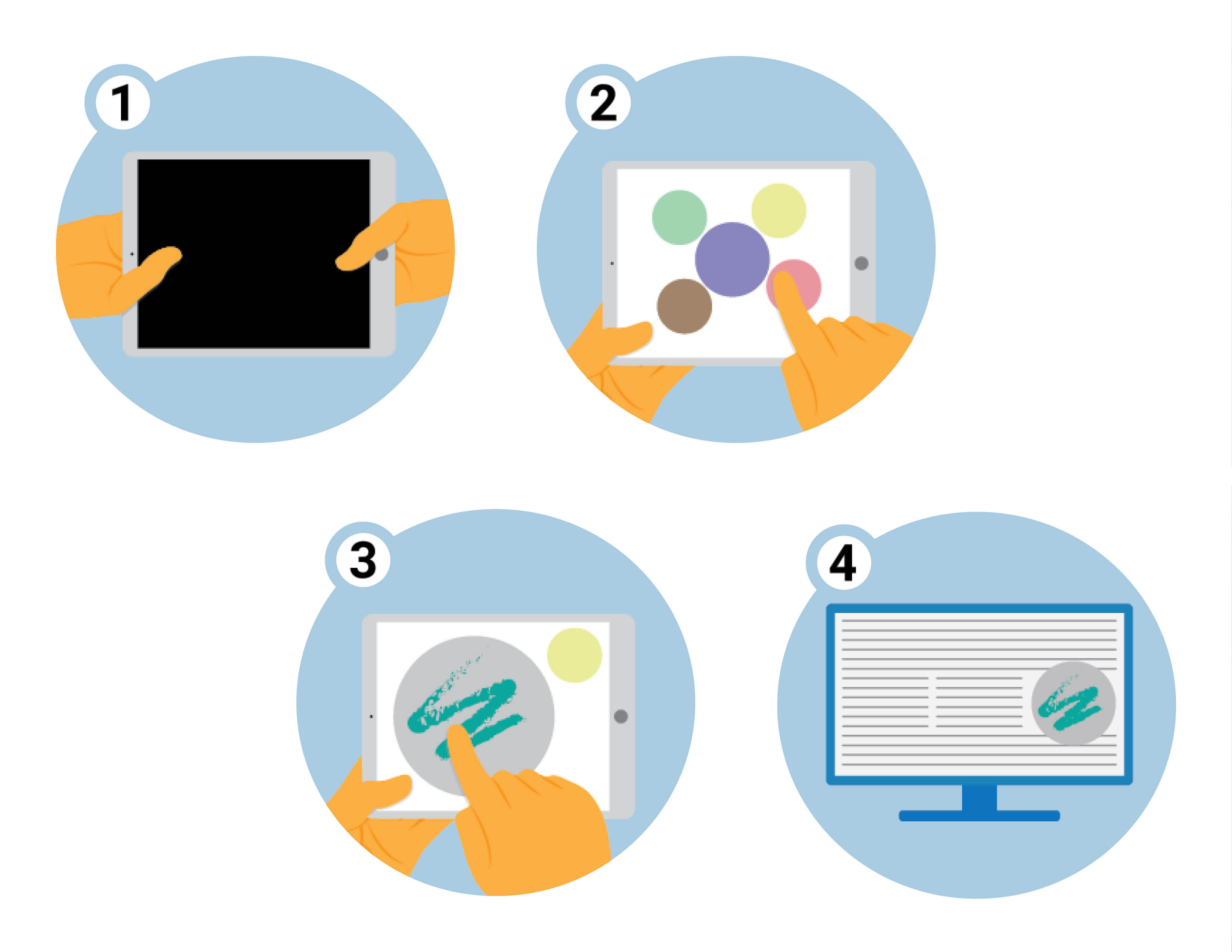
Storyboard
- Patients would be handed an iPad upon entering the clinic room.
- Patient can adjust lighting, change music, and draw illustrations to represent themselves
- Patient can edit an existing drawing or start with a blank canvas.
- The completed drawing will appear on a random section of their electronic health record.
Usability Testing
I gave participants a scenario in which they were sitting on the bed in the clinical room and was handed an iPad with the application before seeing the physician. The majority of them were able to navigate through the interface smoothly, yet some showed confusion about the purpose of this application and the connection between the series of actions.
Narrative
To successfully communicate the purpose of the application turned out to be the most challenging aspect of the prototyping stage. If users knew the real purpose of the drawing, it could affect their willingness to create drawing to truly reflect their individuality and a lengthy explanation can also drive them away from using it. Yet without a reason, it would be difficult to convince them to draw.
After more testing and discussion, I came to the solution of creating separate narrative and purpose for the patients. For patients, this application is not to show their individuality but to show their support for a cause they cared about.